Meritorious Professor
Dr Bader Faiyaz Zuberi
FCPS, MACG (USA), AGAF (USA)
FCPS, MACG (USA), AGAF (USA)
Gastroenterologist & Hepatologist

OMI CLINICS DHA
Off 34th St. Khayaban-e-Bukhari,
DHA Phase-6, Karachi
Monday to Friday
10:00 am to 1:00 pm
Ghulam Mustafa 0302-1496677

ANKLESARIA NURSING HOME
Aga Khan -III Road, Garden
Karachi
Monday to Saturday
3:00 pm to 5:30 pm
3:00 pm to 5:30 pm
Nabi Bux 0309-0573709

OMI HOSPITAL
89/1, Depot Lines
MA Jinnah Road, Karachi
Monday to Friday
6:00 pm to 8:00 pm
6:00 pm to 8:00 pm
Raheem Bux 0334-3229934
RESEARCH PAPERS (RECENT)
Details of research papers of Prof Bader Faiyaz Zuberi published after 2018.
Click on the icon above to view.
Click on the icon above to view.
RESEARCH PAPERS (PREVIOUS)
Details of research papers of Prof Bader Faiyaz Zuberi published before 2018.
Click on the icon above to view.
ENDOSCOPIC VIDEOS
To view procedural videos performed by Prof Bader Faiyaz Zuberi, click the icon above
Prof Bader Faiyaz Zuberi
Prof Bader Faiyaz Zuberi worked as Meritorious Professor (BPS-22), Dean Medicine & Allied Sciences at Dow Medical College, Dow University of Health Sciences (DUHS) Karachi and Consultant Physician and Gastroenterologist Dr Ruth KM Pfau Civil Hospital Karachi. He has served in DUHS in various capacities including Head of Medicine Unit-I, Chairman Department of Medicine, Dean Faculty of Medicine & Director Clinical Trials Unit. He is CPSP approved supervisor for Medicine & Gastroenterology training leading to FCPS Gastroenterology.
Prof. Zuberi has received special training in Gastroenterology from USA, Singapore & Hong Kong and has attended many therapeutic endoscopic workshops in various countries. He has also conducted many workshops on endoscopic procedures and on medical writing and statistical analysis.
He has thrice received "Young Investigators Award" on his research papers and have more than 100 publications in local and international journals to his credit.
Endoscopic Procedures
Prof Zuberi is expert and experienced at performing all endoscopic procedures like Upper GI Endoscopy, Colonoscopy, ERCP, Sclerotherapy, PEG placement, Oesophageal dilatation & Stent Placement, Band ligation of Oesophageal Varices.
Prof Zuberi performs free endoscopic procedures on Monday at DOTS OT Complex, 3rd Floor, Civil Hospital Karachi.
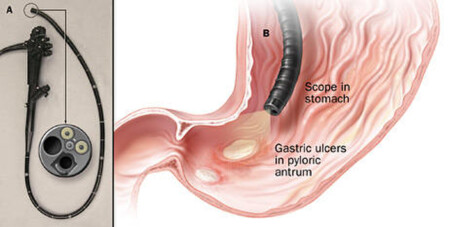

Upper GI Endoscopy
Esophago-gastro-duodenoscopy (EGD) or simply gastroscopy is an endoscopic procedure that allows direct examination of the esophagus, stomach, and duodenum. The examination takes approximately 10 minutes and may be performed as an outpatient in a procedure room, or in a hospital. Upper endoscopy is well tolerated with minimal discomfort. EGD may be used to evaluate abdominal pain, heartburn, persistent nausea or vomiting, swallowing difficulties, upper gastrointestinal bleeding, chest pain in the absence of heart disease or bloody stools. It may also be used for periodic screening, surveillance, to remove foreign bodies or to control bleeding.
Prior to the procedure, the patient is registered and a medical history documented. Then, a needle/catheter is inserted into a vein for intravenous access (allowing for fluid and sedative administration). The throat may be treated with a topical anesthetic to suppress the gag reflex. Pain medication and a sedative may also be administered before the procedure. A plastic mouthpiece is placed between the teeth to prevent damage to the endoscope. As the patient swallows, the endoscope is guided through the esophagus, stomach, and duodenum while the physician examines the mucosa (lining) displayed on a monitor.
Air may be introduced through the endoscope distending the folds of tissue and enhancing the examination. A variety of accessory equipment may be used through the endoscope to obtain tissue biopsies or samples of digestive fluid, which are sent to the laboratory for analysis. At the completion of the examination, the endoscope is withdrawn.
On completion of the examination, the patient is taken to the recovery area. Patients are observed for upto 1 hour until the effects of the medication wear off. The physician will inform the patient about the results of the EGD and provide additional information as needed. Patients are discharged with instructions to have limited activity for the remainder of the day. Patients may experience belching and/or flatulence for the next 24 hours. In addition they may experience some throat discomfort.
Esophagogastroduodenoscopy is safe and effective when performed by professionals with appropriate training and experience. Complications are rare (1 out of 100,000), and may include bleeding, perforation, aspiration, or adverse reaction to the anesthetic or medication. Patients should contact their physician in the event of difficulty swallowing, pain, fever, bloody stools or blood in vomit following their procedure.
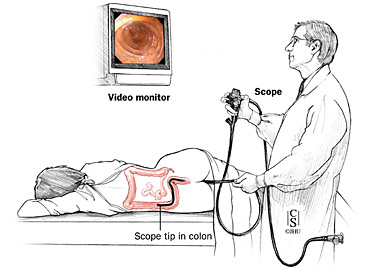
Colonoscopy
Colonoscopy is an endoscopic procedure to directly examine the interior of the large intestine (large bowel) from the rectum to the terminal ileum using a colonoscope. The procedure takes approximately 20–40 minutes and is usually performed as an outpatient. Diagnostic colonoscopy is recommended for alterations in bowel habits, occult or frank blood in the stool, unexplained anemia, and as a screening procedure for colon cancer.
The colon must be completely clean for colonoscopy to be thorough and safe. Patients may be placed on a liquid diet for 1–2 days before the examination and administered oral colonic wash solutions to clear the colon. Patients are asked to arrive at the endoscopy suite about 1–2 hours prior to the procedure and should be accompanied by a responsible adult to transport them home. The patient is registered and a medical history is documented. Then, a needle/catheter is inserted into a vein for intravenous access (allowing for fluid and sedative administration).
The video-camera on the colonoscope transmits images of the inside of the colon to a monitor. Multiple monitors in the endoscopy suite can allow for multiple examiner viewing. After the sedation is administered the physician usually performs a digital rectal exam after which the colonoscope is inserted into the rectum. The colonoscope is advanced to the cecum. During the exam, air may be introduced into the colon to improve visibility. The physician may take biopsies or remove polyps during the procedure using instruments passed through the endoscope. The tissue samples are sent to a laboratory for analysis. If there is bleeding in the colon the physician has a variety of instruments at his disposal to treat bleeding. There is no pain involved with these procedures.
On completion of the examination, patients remain in the recovery area for around an hour until the effects of the medication wear off. The physician will inform the patient about the results of the colonoscopy and provide additional information as needed. Patients are discharged with instructions to have limited activity for the remainder of the day. Walking may help relieve bloatedness or gas.
Colonoscopy is safe and effective when performed by professionals with appropriate training and experience. Complications are rare (1:10,000). Complications may include bleeding from a biopsy site or perforation (a tear in the bowel wall). Symptoms of abdominal pain, distention, nausea, vomiting, chills, fever or rectal bleeding should be reported to the physician.
ERCP
Endoscopic Retrograde Cholangio-Pancreatography (ERCP) is a technique that combines the use of endoscopy and fluoroscopy to diagnose and treat certain problems of the biliary or pancreatic ductal systems. Through the endoscope, the physician can see the inside of the stomach and duodenum, and inject radiographic contrast into the ducts in the biliary tree and pancreas so they can be seen on X-rays. ERCP is used primarily to diagnose and treat conditions of the bile ducts and main pancreatic duct, including gallstones, inflammatory strictures (scars), leaks (from trauma and surgery), and cancer. ERCP can be performed for diagnostic and therapeutic reasons.
The patient is sedated or anaesthetized. Then a flexible camera (endoscope) is inserted through the mouth, down the esophagus, into the stomach, through the pylorus into the duodenum where the ampulla of Vater (the opening of the common bile duct and pancreatic duct) exists. The sphincter of Oddi is a muscular valve that controls the opening of the ampulla. The region can be directly visualised with the endoscopic camera while various procedures are performed. A plastic catheter or cannula is inserted through the ampulla, and radiocontrast is injected into the bile ducts and/or pancreatic duct. Fluoroscopy is used to look for blockages, or other lesions such as stones.
When needed, the opening of the ampulla can be enlarged (sphincterotomy) with an electrified wire (sphincterotome) and access into the bile duct obtained so that gallstones may be removed or other therapy performed. Other procedures associated with ERCP include the trawling of the common bile duct with a basket or balloon to remove gallstones and the insertion of a plastic stent to assist the drainage of bile. Also, the pancreatic duct can be cannulated and stents be inserted. The pancreatic duct requires visualisation in cases of pancreatitis.
The major risk of an ERCP is the development of pancreatitis, which can occur in up to 5% of all procedures. This may be self limited and mild, but may require hospitalization, and rarely, may be life-threatening. Patients at additional risk for pancreatitis are younger patients, patients with previous post-ERCP pancreatitis, females, procedures that involve cannulation or injection of the pancreatic duct, and patients with sphincter of Oddi dysfunction.
Oversedation can result in dangerously low blood pressure, respiratory depression, nausea, and vomiting. There is also a risk associated with the contrast dye in patients who are allergic to compounds containing iodine. Other complications (less than 1 per 10,000) may include; heart and lung problems, bleeding after sphincterotomy, infection in the bile duct (cholangitis) and perforation (a tear in the intestine).
The patient is sedated or anaesthetized. Then a flexible camera (endoscope) is inserted through the mouth, down the esophagus, into the stomach, through the pylorus into the duodenum where the ampulla of Vater (the opening of the common bile duct and pancreatic duct) exists. The sphincter of Oddi is a muscular valve that controls the opening of the ampulla. The region can be directly visualised with the endoscopic camera while various procedures are performed. A plastic catheter or cannula is inserted through the ampulla, and radiocontrast is injected into the bile ducts and/or pancreatic duct. Fluoroscopy is used to look for blockages, or other lesions such as stones.
When needed, the opening of the ampulla can be enlarged (sphincterotomy) with an electrified wire (sphincterotome) and access into the bile duct obtained so that gallstones may be removed or other therapy performed. Other procedures associated with ERCP include the trawling of the common bile duct with a basket or balloon to remove gallstones and the insertion of a plastic stent to assist the drainage of bile. Also, the pancreatic duct can be cannulated and stents be inserted. The pancreatic duct requires visualisation in cases of pancreatitis.
The major risk of an ERCP is the development of pancreatitis, which can occur in up to 5% of all procedures. This may be self limited and mild, but may require hospitalization, and rarely, may be life-threatening. Patients at additional risk for pancreatitis are younger patients, patients with previous post-ERCP pancreatitis, females, procedures that involve cannulation or injection of the pancreatic duct, and patients with sphincter of Oddi dysfunction.
Oversedation can result in dangerously low blood pressure, respiratory depression, nausea, and vomiting. There is also a risk associated with the contrast dye in patients who are allergic to compounds containing iodine. Other complications (less than 1 per 10,000) may include; heart and lung problems, bleeding after sphincterotomy, infection in the bile duct (cholangitis) and perforation (a tear in the intestine).
Email
Response time may be up to a week. Please note that no professional advise will be given on email, for that kindly visit any of the clinics. Daily 2.5% of patients are seen free from Zakat, request for free consultation if Zakat eligible.



